Glycated Hemoglobin, commonly known as HbA1c, is a crucial biomarker in the world of diabetes management. It plays a pivotal role in assessing long-term blood sugar control and is widely used by healthcare professionals to monitor and manage diabetes. This article explores the significance of glycated hemoglobin, its formation, understanding and its implications for individuals living with diabetes.
Hemoglobin is a protein found in red blood cells responsible for transporting oxygen from the lungs to various tissues and organs throughout the body. When glucose in the blood binds to hemoglobin, a process known as glycation occurs. This binding is irreversible and forms glycated hemoglobin, HbA1c. The higher the blood glucose levels over time, the greater the percentage of glycated hemoglobin.
Glycated hemoglobin is an essential tool in diabetes management because it reflects average blood glucose levels over the past two to three months.
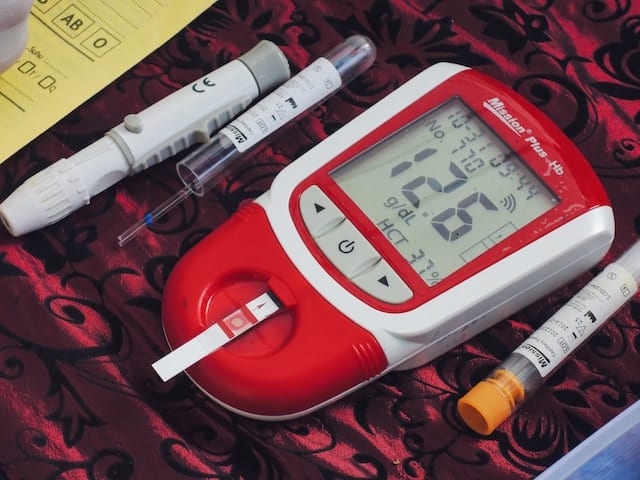
While daily self-monitoring with blood glucose meters provides real-time information, HbA1c offers a broader picture of a person’s overall blood sugar control. This long-term perspective is valuable for healthcare professionals to make informed decisions about treatment plans and adjustments.
For individuals with diabetes, maintaining optimal glycated hemoglobin levels is crucial in preventing complications associated with high blood sugar. The American Diabetes Association recommends a target HbA1c level of below 7% for most adults with diabetes. However, individualized targets may vary based on factors such as age, health status, and the presence of other medical conditions.
Regular monitoring of HbA1c levels is integral to managing diabetes effectively. Healthcare providers typically recommend testing every three to six months to assess the effectiveness of the current treatment plan. Additionally, glycated hemoglobin levels play a significant role in the diagnosis of diabetes. A high HbA1c level, along with other diagnostic criteria, can confirm the presence of diabetes or prediabetes.
While glycated hemoglobin is a valuable marker, it’s essential to recognize its limitations. HbA1c may not accurately represent blood sugar control in certain situations, such as during rapid changes in blood glucose levels. Conditions affecting red blood cells, such as anemia or certain hemoglobin variants, can also impact the accuracy of HbA1c measurements. In such cases, healthcare providers may rely on alternative methods of assessing glycemic control.
Achieving and maintaining optimal HbA1c levels involves a multifaceted approach. Lifestyle factors, including a healthy diet, regular exercise, and weight management, contribute significantly to blood sugar control. Medications, such as oral hypoglycemic agents or insulin, may also be prescribed to help regulate blood glucose levels. The synergy of lifestyle modifications and medication is key to successful diabetes management and achieving target HbA1c levels.
In conclusion, glycated hemoglobin serves as a valuable tool in the management of diabetes. This biomarker offers a comprehensive view of blood sugar control over an extended period, guiding healthcare professionals in tailoring effective treatment plans. Regular monitoring of HbA1c levels, coupled with lifestyle modifications and appropriate medications, empowers individuals with diabetes to take control of their health and reduce the risk of complications. Understanding the significance of glycated hemoglobin is a crucial step towards achieving optimal diabetes management and improving overall well-being.
Image CreditI’m a type 1 diabetic with diabetes knowledge in t1d and t2d, as well as nutrition and low-carb keto diet information, fitness and exercise programs to help keep you in optimal diabetes health. Take advantage of our diabetic health tools for a healthier lifestyle!
This website uses cookies.