The A1C calculation estimates the percentage of hemoglobin in the bloodstream bonded with glucose. This is an indicator for average blood sugar levels for the prior 2 to 3 months, and this is where the hemoglobin A1C calculator #a1ccalculator or a1c converter comes into play.
For example, one might experience elevated glucose levels at night without realizing it. The introduction of A1C evaluations in the 1980s revolutionized diabetes management and provided a more comprehensive picture of glucose control. Learn more about the glucose a1c conversion methods on this page, along with our conversion chart below.
Why is it Important to Get a Hemoglobin A1C Test?
A Hemoglobin A1C test provides the mean blood glucose levels for the preceding two to three months. Therefore, it offers insights into glucose control regardless of temporary variations in fasting glucose levels. Consequently, an A1c average calculator is indispensable for diagnosing and monitoring prediabetes and diabetes.
A1C evaluates the glucose-bound hemoglobin percentage, which reflects the average glucose levels for three months (the average lifespan of hemoglobin cells). This period is critical as it assesses the historical data on glucose levels and gives us a broader perspective on glucose management over time.
How the A1C Calculator Works?
To use an A1C calculator, you will need to have your A1C test results, which are typically given as a percentage. The calculator will then estimate your average blood sugar levels based on this percentage. The American Diabetes Association (ADA) has established the following general guidelines for A1C levels:
- Less than 5.7%: Normal blood sugar control
- 5.7% to 6.4%: Prediabetes
- 6.5% or higher: Diabetes
It’s important to note that individual target A1C levels may vary based on factors such as age, overall health, and the presence of other medical conditions. Your healthcare provider can help determine your specific target A1C level and provide guidance on achieving it.
The HbA1c tool calculates your average blood glucose level in (mg/dl) units. The glycated Hemoglobin A1C test shows your average blood sugar level over the past 2 to 3 months. If you’d like to know your average blood sugar level over that time frame, enter your most recent (glycated Hemoglobin test) HbA1c results into the A1C calculator below for instant eAG results.
How Can I Calculate My A1C?
Additionally, you can calculate your A1c level by entering your average blood sugar level into that field and hitting enter for your result. In order to use the tool as a glucose to a1c calculator (find your average bg level in your glucometer history). So basically, when people ask, “Can I calculate my A1C at home?“ – the answer is yes. Reference the A1C chart with your result value. A helpful tool for diabetics with t1d or t2d diabetes!
We use this formula 28.7 X A1C – 46.7 = eAG, which is the affiliation between A1C and eAG (average glucose). Additionally, we use this unit converter for all our conversion calculators.
Hemoglobin A1C Calculator Tool
A1C Value Result
Average Blood Sugar Result
- Important Note: The tool should not be used in place of a lab A1C test or to make treatment changes. Consult with your healthcare provider.
- For a complete understanding of your overall diabetes management plan, always discuss any results or additional information from this tool with your healthcare provider. The chart and calculation are not intended for therapy decisions or to replace professional medical advice.
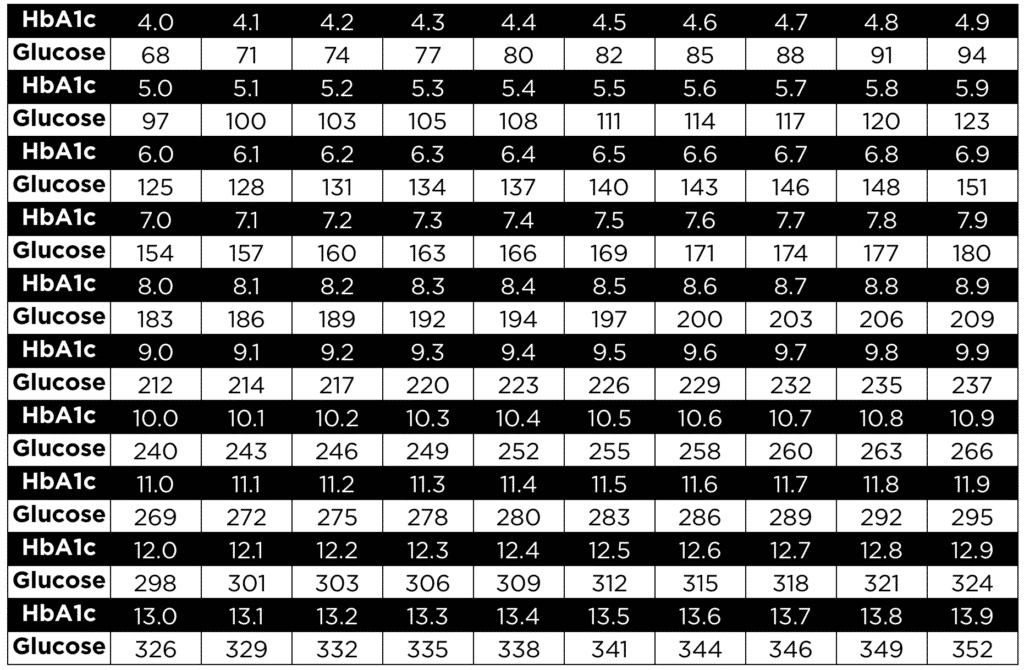
HbA1c Blood Sugar Conversion Chart
The HbA1c blood sugar conversion chart below estimates average blood glucose based on your HbA1c and vice versa. You can see that under each A1c value, there is an approximate blood glucose (bg) level. For instance, if your A1c is 5.1%, your average blood glucose level is 100 mg/dL.
Conversely, you can estimate your HbA1c from an average blood glucose. A diabetic patient with an average blood glucose level of 200 mg/dL will have a HbA1c of 8.6%. The glucose A1c conversion chart below maps out your results. Also, try the A1C level calculator above for more accurate results.
Calculation of the Hemoglobin A1C Measurement
- A1c Calculator (a1c converter) uses average blood sugar input
- Accuracy improved by averaging several fasting blood sugar measurements over 2-3 months
Can You Have a “Normal” A1C Even With Blood Sugar Swings?
It’s possible for someone to end up with an A1C result that appears well-managed, even if their day-to-day blood sugar is often on a roller coaster. This is because the A1C is an average—it reflects the typical blood glucose over the past 2–3 months, but not the ups and downs that might happen throughout each day.
If you experience frequent highs and lows, these can “average out,” leading to an A1C that looks like you’re in the target range. However, relying on A1C alone can be misleading for some people. That’s why frequent self-monitoring with a glucometer is so important. Fingersticks or continuous glucose monitoring (CGM) devices, such as those from Dexcom or Abbott, provide a clearer picture of your real-time blood sugar patterns—capturing both spikes and drops.
For optimal glucose management, combine your A1C result with regular self-checks. This approach will help you and your healthcare provider understand both your long-term averages and your daily variability.
Understanding Your A1C Test Results
Deciphering your A1C results involves grasping the guidelines and your personal target range. Here’s a breakdown of what each range might signify:
- Below 5.7%: Reflects normal blood sugar control, indicating managed blood sugar levels.
- 5.7% to 6.4%: This range hints at prediabetes, signifying blood sugar levels higher than normal but not yet in the diabetes zone. It’s a period to consider lifestyle adjustments to prevent or delay the onset of diabetes.
- 6.5% or above: Indicates diabetes denoting elevated blood sugar levels that may necessitate medication, dietary changes, and lifestyle modifications for management.
It’s crucial to note that while the A1C test provides insight into your blood sugar control, it should not replace daily monitoring. Instead, it complements monitoring efforts and offers a more comprehensive view of your overall blood sugar management.
Why Daily Self-Monitoring Still Matters
The A1C test gives a long-term average of your blood sugar over the past two to three months, but it doesn’t reveal the daily highs and lows. Regular self-checks—like fasting, post-meal, and bedtime glucose measurements—are essential for understanding how specific foods, activities, medications, or stress affect your blood sugar in real time. Without these daily checks, your A1C might look deceptively “in range,” even if you experience frequent spikes and drops.
Blending Long-Term and Day-to-Day Results
To get the clearest picture of your glucose control, use your daily readings alongside your A1C results. Together, they help you and your healthcare provider pinpoint patterns, spot problem areas, and make better decisions about your care plan. This combined approach leads to more effective diabetes management and fewer surprises along the way.
What’s a Normal Hemoglobin A1C Test Result?
Reiterating the above interpretation, normal A1C levels are below 5.7 percent. Numbers between 5.7% and 6.4 percent indicate prediabetes and levels above 6.5% signify diabetes. Regular A1C testing is recommended biannually or more often, depending on individual circumstances. Luckily, our A1c Calculator will reduce the need to get tested in the laboratory.
How Accurate are the A1C Results?
The accuracy of the A1C Calculator is very high, as recommended by the ADA. Of course, it cannot replace the actual blood test. However, it still provides valuable insights and results for free!
Who should use the A1C Calculator?
The A1c Calculator is recommended for adults, or younger individuals at risk, due to factors like obesity, history of gestational diabetes, or prediabetes. Elevated A1C levels signal poorly managed diabetes and increase the risk for various health complications.
The benefits of the A1C Tool
An A1c calculator is an invaluable tool for individuals who struggle with diabetes or those at risk. It offers a range of benefits that contribute significantly to effective diabetes management and overall health.
Easy to access
With the advent of online and mobile A1c calculators, individuals can easily access this tool anytime and anywhere. This makes it easier to stay on top of diabetes management without constant visits to the healthcare provider.
Why is the A1C Calculator showing elevated results?
The reason why the A1c calculator might show an abnormal or elevated result could be benign, or it could indicate diabetes. Depending on your age, risk factors, and family history, this could either mean you have type 1 or type 2 diabetes.
Let’s quickly go through the common types of diabetes that elevate your result on the A1c Calculator:
Type 1 diabetes
Formerly referred to as juvenile diabetes, type 1 diabetes (T1D) is commonly seen in children and younger adults.
According to a longitudinal study published by BMC, the annual incidence rate of type 1 diabetes is 34.3 per 100,000 persons for ages 0–19 years and 18.6 per 100,000 persons for ages 20–64 years. As you can see, the incidence is much higher in younger people, hence the old terminology of this disease. This type is classified as an autoimmune disease since the active destruction of the pancreatic tissue erases the beta cells responsible for insulin secretion.
What causes type 1 diabetes?
The complete pathophysiology of type 1 diabetes is not yet understood; however, it involves a type IV hypersensitivity reaction against the pancreas.
In other words, the immune system launches an inflammatory reaction that recruits immune cells like neutrophils, macrophages, and T-cells to destroy the pancreas’s parenchyma (tissue).
Interestingly enough, this reaction is so specific that only the beta cells of the pancreas are damaged; other cells, such as alpha cells, which produce glucagon (hyperglycemic hormone), and the exocrine glands that secrete digestive enzymes are intact!
This destruction is chronic and may take some time before any clinical symptoms are apparent. The final result is a severe insulin deficiency, which leads to chronic hyperglycemia that requires insulin therapy.
The cause behind the autoimmune reaction is still unknown, but researchers believe it’s a combination of nature and nurture.
The nature part involves the genetic predisposition of patients with a family history of type 1 or type 2 diabetes. Also, patients who have other autoimmune diseases such as asthma, inflammatory bowel syndrome (e.g., Crohn’s disease, ulcerative colitis), and multiple sclerosis are at a higher risk of developing type 1 diabetes.
The nurture part is believed to be some environmental trigger that launches the immune reaction. The suspected trigger could be a viral infection, exposure to certain toxins, and even dietary choices.
Together, these two entities create the perfect environment to develop type 1 diabetes.
Type 2 diabetes
Type 2 diabetes (T2D) is similar to type 1 when it comes to signs and symptoms; however, the pathophysiology is entirely different.
For starters, the pancreas is entirely intact, and insulin secretion is not altered. Moreover, there is no autoimmune component of type 2 diabetes, and the risk factors are different.
T2D is commonly seen in heavier individuals above the age of 40 with multiple risk factors for diabetes.
The main issue of T2D is that the cells become resistant to insulin’s action; in other words, insulin is readily available in the bloodstream, but when it arrives at the cell and tries to signal it so that glucose can enter, there is no response.
This was believed to be the only mechanism of type 2 diabetes. However, recent research shows that patients with T2D eventually develop relative insulin deficiency via the active destruction of the pancreatic tissue. Note that the range of destruction is nowhere near that of type 1 diabetes, but it does exist.
The combination of insulin resistance and its relative deficiency is the cornerstone of diabetes pathophysiology.
What causes type 2 diabetes?
It is still unclear why some people develop T2D while others do not, even if both groups have the same risk factors. Nevertheless, we can partially explain using the “nature and nurture” concept. In this case, however, and unlike type 1 diabetes, the nurture part plays the most crucial role.
If you have a family history of T2D, your risk of developing the disease is way higher than someone who doesn’t, and that’s the natural part.
The nurture part involves many risk factors, including obesity, sedentary life, and being diagnosed with a gynecological condition known as polycystic ovarian syndrome (PCOS). However, the most critical risk factor is, by far, obesity.
Eating multiple meals high in refined sugar and trans-fat daily stimulates your pancreas to secrete insulin several times daily.
This effect is accentuated by the fact that most sugars found in fast and processed foods are simple sugars with a high glycemic index.
The glycemic index is the rate at which a particular food raises your blood sugar levels after consuming it. For instance, juice and Coke have the highest glycemic index since they are mainly composed of simple sugars.
On the other hand, oatmeal and lentils have a shallow glycemic index.
To summarize, consuming foods with a high glycemic index stimulates the pancreas multiple times daily, increasing insulin levels in a fluctuating pattern.
Eventually, this overstimulation of the cells by insulin will lead to insulin resistance and type 2 diabetes.
Elevated A1c Blood Glucose Test? Here are the risk factors
Family history
Researchers found that having a family member with diabetes increases your risk of developing elevated hemoglobin A1c measurement levels.
Moreover, some genes were identified to play a role in the increased risk of diabetes incidence between the members of one family.
Age
Type 2 diabetes is seen more over the age of 40-45. However, with the spread of the obesity epidemic over the past decade, the incidence of T2D in younger adults and teenagers is on the rise.
Race
Diabetes is more common in African-Americans and Asian Americans compared to white people than in other ethnic groups. This adds more evidence to the genetic part of diabetes.
Atopy
Atopy is an immunological state that describes people predisposed to developing autoimmune and inflammatory conditions.
For example, a patient who has allergic rhinitis, atopic dermatitis, and Crohn’s disease is more likely to develop other autoimmune diseases because their immune system is already out of whack and ready to attack new body tissues when the opportunity comes.
Obesity
As we’ve mentioned earlier, this is the most crucial risk factor for T2D, and the more fat tissue you have, the more resistant your cells will become.
Polycystic ovarian syndrome
PCOS is a gynecological condition characterized by multiple cysts spread all over the ovaries and increased insulin resistance. If left untreated, this condition may eventually lead to full-blown diabetes.
Early Signs and symptoms of elevated A1c Levels
If the A1c Calculator shows elevated levels, you may experience some symptoms. The signs and symptoms of T2D are the same as those of type 1 diabetes.
Here are some of the signs and symptoms of diabetes:
- Feeling hungry all the time
- Fatigue
- Excessive thirst
- Polyuria
- Dry mouth
- Itchy skin
Creating a Scenario to Explain the Signs and Symptoms of Diabetes
To explain the signs and symptoms of diabetes, we will create a scenario.
You wake up, shower, and prepare your favorite breakfast meal. After breakfast, all the food is digested in your stomach and small intestines; this involves the breakdown of the three primary macronutrients (e.g., protein, fat, and carbohydrates) and their absorption into the bloodstream.
Your blood sugar will rise after a few minutes of eating. Due to high blood sugar, the pancreas secretes insulin to lower blood glucose levels to normal ranges (below 100 mg/dl).
That is the physiological process that happens after each meal. Let us now remove insulin from the equation.
Because type 1 diabetes is characterized by destroying the cells responsible for insulin secretion, we don’t have a method for reducing blood sugar levels.
Subsequently, your cells cannot get any glucose inside and start sending signals to your brain to stimulate hunger, making you eat more.
As you do that, blood sugar will get even higher, and water will start moving from inside the cells to blood vessels because of the different osmotic gradient. Now you have more volume in your blood vessels, so the kidneys have to filter more fluid, and you will start urinating excessively.
When you lose excessive fluids in the urine, the hypothalamus will stimulate the thirst response, and you will begin to drink water in large amounts.
Et voila! The classical triad of diabetes is hyperphagia (excessive eating), polyuria (excessive urination), and polydipsia (extreme thirst).
In addition, the inability of glucose to get inside the cells will make you feel lethargic (fatigued) and cause substantial weight loss in a short period.
Risks Associated with High A1C Levels
Health Complications
Having A1C levels can lead to health complications. It raises the chances of developing type 2 diabetes, heart conditions, and stroke. Additionally, it can damage the blood vessels, kidneys, and eyes.
Furthermore, increased A1C levels are linked to nerve damage (Diabetic neuropathy) that can result in tingling sensations or loss of feeling in the feet. This is concerning because individuals with high A1C levels often face difficulty healing foot ulcers or infections.
Long Term Risks
Sustained elevation of A1C levels raises the chances of developing conditions such as kidney disease and vision problems. Over time, these health concerns may negatively impact quality of life.
Additionally, individuals with controlled blood sugar levels are less susceptible to decline than those with uncontrolled glucose levels. This suggests that elevated A1C values could affect brain function as time progresses.
Keeping your A1C levels within a healthy range can offer a host of protective benefits. Not only does it help reduce the risk of long-term complications like nerve problems, kidney disease, and heart issues, but it also aids in safeguarding your vision. By managing your A1C effectively, you lower the chances of developing diabetic neuropathy, eye damage, and cardiovascular concerns—all of which can significantly impact quality of life over time.
Try out our other health tools to help you better manage blood sugar levels and weight management!
