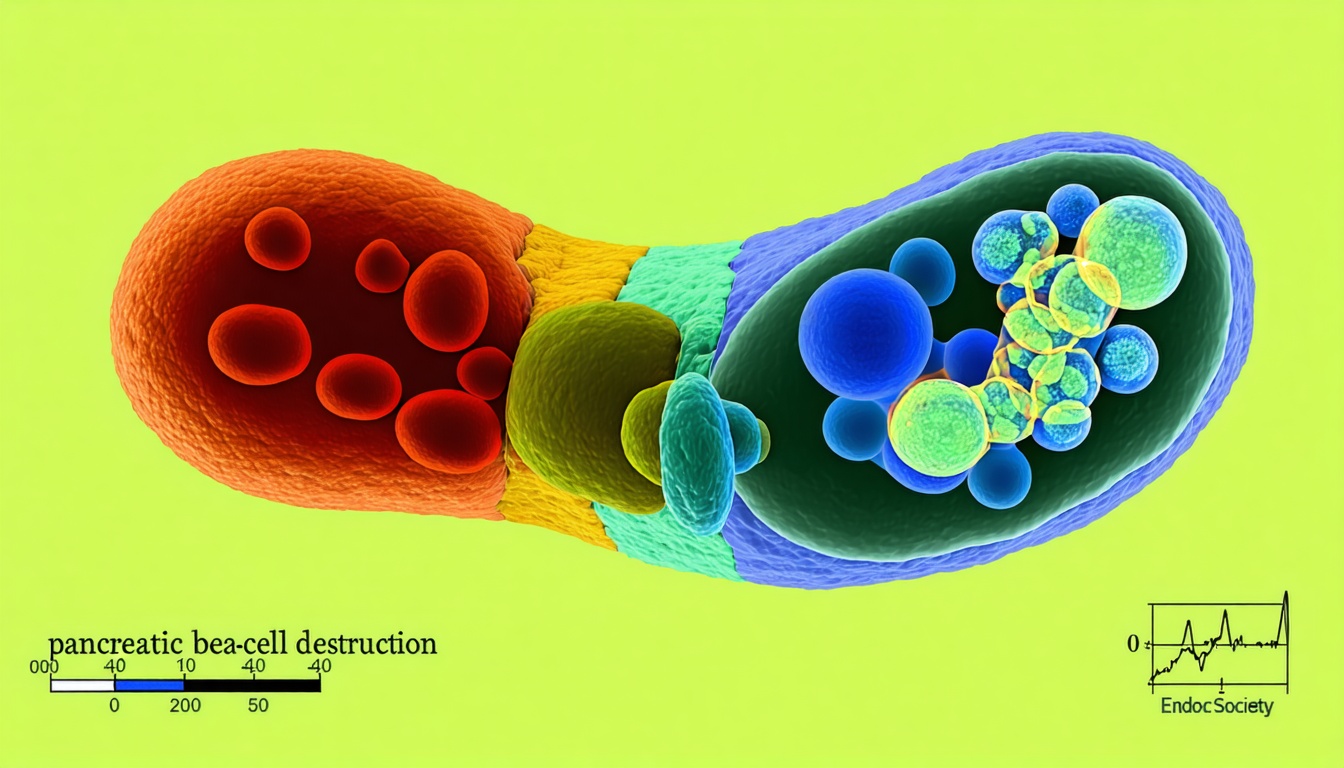
Understanding Pancreatic Beta-Cell Destruction in T1D
Pancreatic beta-cell destruction is a defining feature of type 1 diabetes (T1D), where the immune system mistakenly attacks and destroys insulin-producing cells in the pancreas. According to the Endocrine Society’s Scientific Statement, T1D can arise in childhood as well as adulthood, but many questions remain about how these cells are lost, why the disease presents differently in various individuals, and how interventions may prevent or delay its progression (Endocrine Society).
Examine The Immune Mechanism
T1D develops when the immune system targets beta cells (insulin-producing cells) inside the pancreatic islet. This gradual autoimmune attack often begins with the formation of autoantibodies that recognize proteins associated with beta cells, such as insulin itself or glutamic acid decarboxylase. In many cases, these autoantibodies appear years before clinical T1D emerges. Individuals who produce multiple autoantibodies are at a higher risk of progressing to a stage where they require insulin therapy to control blood glucose (Medscape).
Recognize Knowledge Gaps
The Endocrine Society’s statement highlights notable gaps in understanding the pathogenesis (origin and development) of T1D:
- Genetic factors that contribute to disease risk
- Variations in the immune response that lead to different rates of pancreatic beta-cell destruction
- Early events that precede autoantibody formation
Adding a proposed Stage 0 to the widely used disease model could help researchers investigate the earliest triggers. This approach may lead to improved screening and the discovery of therapies that halt beta-cell damage before blood glucose becomes difficult to regulate (Endocrine Society).
Identify Heterogeneity In Adults
Although T1D is often associated with childhood onset, roughly 40% of cases may develop after age 30. In these individuals, the loss of beta cells can progress slowly, which sometimes results in a misdiagnosis of type 2 diabetes. The Endocrine Society’s statement points to a need for better diagnostic criteria, so adults with new-onset T1D receive proper care. Slower progression involves more subtle warnings that can be missed until significant insulin deficiency prompts classical T1D symptoms (Medscape).
Review Emerging Therapies
Investigational treatments aim to preserve beta-cell function and delay the need for insulin. One example is teplizumab (sold as Tzield), an immunotherapy shown to postpone clinical T1D by targeting the early autoimmune response. This therapy demonstrates the potential value of screening individuals with a family history of T1D or the presence of specific autoantibodies. Specialists call for more research into therapy combinations, along with population-based screening, to identify risk factors and tailor interventions before irreversible cell loss occurs (source).
Below is a brief overview of the established stages of T1D, along with the newly proposed Stage 0:
| Stage | Characteristics |
|---|---|
| 0 (Proposed) | Pre-autoantibody events not well understood |
| 1 | Presence of autoantibodies, normal blood glucose |
| 2 | Presence of autoantibodies, mild disturbances in blood glucose |
| 3 | Overt T1D, noticeable symptoms, insulin requirement |
Key Takeaways
- The immune system’s targeting of pancreatic beta cells underlies the development of T1D.
- Researchers have proposed adding a Stage 0 to capture early factors that might trigger autoimmunity.
- Adult-onset T1D is more common than previously thought, and slow progression can lead to misdiagnosis.
- Therapies like teplizumab highlight the importance of screening for early T1D markers.
By exploring these under-researched aspects of T1D, the scientific community can develop more targeted diagnostic tools and treatment options to preserve beta-cell function and improve outcomes for individuals with this autoimmune condition. Learn more about knowledge gaps in T1D!





Leave a Reply