Adjusting Diabetes Medications for Exercise: How Golfers Can Avoid Highs and Lows
Managing diabetes can often feel like navigating a complex puzzle, but exercise can be a powerful tool to simplify the process. Not only does physical activity help control your blood sugar levels in the moment, but it also delivers long-term benefits like improved insulin sensitivity and reduced risk of complications. Additionally, adjusting diabetes medications for exercise and golf is beneficial to avoid sugar highs and lows. Read on to learn more!
Golf in particular is a wonderful form of exercise for diabetics. It’s low-intensity, engages major muscle groups, and relieves stress, all helpful for stabilizing blood sugar levels. If you’re planning on increasing your exercise, here’s how to incorporate exercise into a diabetic-friendly lifestyle.
Diabetes and Exercise: The Link
Exercise plays a surprising role in managing diabetes by directly affecting blood glucose levels. Here’s how it works:
Increased Insulin Sensitivity:
- When you exercise, your muscle cells use glucose for energy, improving the effectiveness of insulin and reducing blood sugar levels. This effect can last 24 hours or more after physical activity.
Direct Glucose Uptake:
- Contracting your muscles can absorb glucose from the blood, even without insulin, which helps to stabilize your blood sugar during and after exercise.
Long-Term Benefits:
- Regular physical activity lowers HbA1C levels (a measure of long-term glucose control) and reduces the risk of complications associated with diabetes.
The Specific Effects of Golf
Golf is characterized by moderate, intermittent activity and mental focus, which can actually offer unique benefits for diabetics:
Physical Activity:
- Walking between holes and swinging your golf clubs both engage major muscle groups, which promote glucose usage and improve insulin sensitivity.
Low-Intensity Exercise:
- Golf’s moderate intensity is ideal for maintaining steady glucose levels, avoiding the spikes or drops seen with high-intensity activities.
Mental Focus:
- Concentrating on gameplay can reduce stress, indirectly benefiting blood sugar regulation. Stress hormones can influence glucose levels, so engaging in stress-relieving activities makes a big difference.
Golf is a safe, accessible activity for many diabetics and provides a mix of physical and mental health advantages. But as always, consult your healthcare provider before adjusting your diabetes medications for exercise, golf or starting new exercise routines, especially if you’re actively managing diabetes.
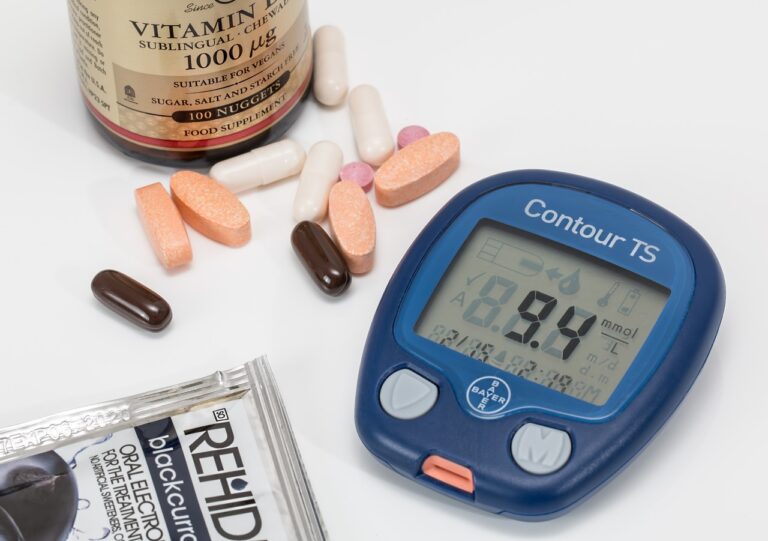
Types of Diabetes Medications
Exercising with diabetes can vary depending on which medication you’re on. Here’s a quick guide to how different medications react to exercise.
Insulin
- Usage: Used primarily for Type 1 diabetes and sometimes Type 2. Helps regulate blood sugar by replacing or supplementing the body’s insulin production.
- Interaction with physical activity: Exercise can increase insulin sensitivity, reducing the dosage you need. But it may also lead to accidental hypoglycemia, so monitoring your blood sugar is even more important when exercising.
Metformin
- Usage: A first-line medication for Type 2 diabetes. It decreases glucose production in the liver and improves insulin sensitivity.
- Interaction with physical activity: Enhances the benefits of exercise by supporting blood sugar control. There’s no significant risk of hypoglycemia when used alone.
Sulfonylureas (e.g., glimepiride, glyburide)
Usage:
- Stimulate the pancreas to release more insulin.
Interaction with physical activity:
- Increases the risk of exercise-induced hypoglycemia, so be careful. Carb snacks may be needed before or after workouts.
SGLT2 Inhibitors (e.g., canagliflozin, dapagliflozin)
Usage:
- Promote glucose excretion through urine.
Interaction with physical activity:
- May cause dehydration or urinary infections, especially during prolonged or intense exercise. Caution advised for high-intensity exercise.
GLP-1 Receptor Agonists (e.g., semaglutide, liraglutide)
Usage:
- Enhance insulin secretion and slow digestion.
Interaction with physical activity:
- Generally safe with exercise and may complement weight management.
Thiazolidinediones (e.g., pioglitazone)
Usage:
- Improve insulin sensitivity in muscle and fat tissues.
Interaction with physical activity:
- Rarely affects exercise response but may contribute to fluid retention during strenuous activity.
Adjusting Diabetes Medications for Exercise
Exercise has a big impact on your blood glucose levels, which means if you’re going to be working out regularly, you’ll probably need some thoughtful adjustments to your diabetes medications. Strategies vary based on the type of diabetes, the medications used, and the nature of the exercise.
We know that golfers don’t just exercise on the golf course, so treat it differently if you’re swinging your golf clubs on the course, on the driving range, or hitting the gym. Consider how intense an exercise session you’re about to have and judge your medication based on that.
Medication Timing and Types
Insulin Users:
- Short-acting insulin: Reduce by 50% if you’re exercising 90 minutes post-meal or near peak activity.
- Long-acting insulin: Maintain usual dose but monitor for delayed hypoglycemia.
Pump Users
- Lower basal rates by 50 to 80% or suspend delivery for aerobic activities. Resume normal rates after exercise.
Oral Medications
- Those on sulfonylureas or meglitinides should monitor closely for hypoglycemia. Non-hypoglycemic agents usually need no dose changes for exercise.
Pre-Exercise Preparations
Whether you’re golfing, getting your cardio in, or doing resistance training, preparing yourself properly beforehand can make a big difference to your safety.
- Blood Glucose Checks: Make sure levels are in a safe range before playing (90 to 250 mg/dL). If levels are low, consume 15 to 30 g of fast-acting carbohydrates.
- Medication Adjustments:
-
Reduce or skip rapid-acting insulin for meals close to activity.
-
Adjust basal rates on pumps 30–60 minutes before exercise.
- Timing Medications: Plan insulin or oral medications to align with the start of activity to avoid peaks during intense play.
During Your Exercise
Even if your medication is “exercise safe”, and you adjust your diabetes medications for exercise, pay close attention to how you feel throughout your session. Being aware is the first step to staying safe and understanding how your body reacts in different situations, eg. in warmer weather, at different times of day, etc.
- Monitoring: Check your blood sugar every 30 minutes if possible, especially during prolonged activity (like golf).
- Symptoms to Watch: Be alert for signs of hypoglycemia (shakiness, confusion) or hyperglycemia (thirst, fatigue).
- Management:
-
Carry fast-acting carbohydrates (eg. glucose tablets, juice) for quick fixes.
-
Avoid high-fat snacks, because they slow glucose absorption.
Post-Exercise Adjustments
Once you’ve gotten through your exercise without a hitch, don’t stop there. Here’s how to set up yourself for a healthy day after your exercise.
- Post-Exercise Monitoring: Check blood sugar immediately after exercise and periodically for 4 to 8 hours due to the risk of delayed hypoglycemia.
- Medication Adjustments: Resume your typical doses but monitor for nighttime lows; consider reducing basal insulin slightly.
- Balanced Meal: Eat a meal with a mix of carbohydrates, protein, and fats to stabilize your blood glucose.
Nutritional Advice for Golfers: Before, During, and After Golf
Planning on hitting the golf course and adjusting your diabetes medications for golfing, but worried about your blood glucose levels? Here’s our advice for keeping yourself healthy and strong, before, during, and after your round.
Before Golf
- Eat a balanced meal an hour or two before your game, including complex carbohydrates (eg. oatmeal or whole-grain bread), lean protein (eg. turkey or eggs), and healthy fats (eg. avocado or egg yolks). This combination will give you sustained energy without sluggishness. Include water or a low-sugar beverage for hydration.
During Golf
- Keep your energy levels stable with snacks like trail mix, fruits (eg. bananas or raisins), or low-sugar energy bars. Sip water consistently or consider electrolyte drinks in hot weather.
After Golf
- Focus on recovery by consuming a mix of protein and carbohydrates within 30 minutes of your game ending. Good options include a turkey sandwich, protein shakes with fruit, or Greek yogurt with granola. Rehydrate with water and electrolyte drinks.
Hydration Strategies
- Don’t wait until you’re thirsty, regularly sip water throughout the game. For extra hydration when it’s hot, add electrolyte tablets to your water or eat hydrating foods like oranges or cucumbers.
Safety Tips and Emergency Preparedness
- Take a bit of time to understand the golf course’s emergency protocols and locations of first aid kits or medical staff. It’s a good idea to make them aware of your condition upfront—just in case you do need extra help.
- In case of dehydration, low blood sugar, or heat-related issues, take breaks in shaded areas and rehydrate promptly. Symptoms like dizziness, nausea, or confusion may require fast action.
Essential Items to Carry in Your Golf Bag
-
Glucose tablets or high-carb snacks for quick energy.
-
Water or electrolyte drinks to stay hydrated.
-
Emergency contact information.
When to Seek Medical Help
Seek help if symptoms of dehydration, heat exhaustion, or hypoglycemia persist despite staying hydrated and snacking. Severe symptoms, like fainting, chest pain, or shortness of breath, should be treated as an emergency.
Conclusion
Living with diabetes takes mindful planning, but it doesn’t mean giving up the activities you enjoy—like a good round of golf. By understanding how different types of exercise and diabetes medications interact, you can safely integrate physical activity into your routine to enhance blood sugar control and overall well-being. Just be sure to check with your healthcare pro before adjusting your diabetes medications for exercise.
Whether you’re hitting the links or engaging in other exercises, proper preparation, ongoing monitoring, and balanced nutrition are the pillars of health in this case. Embrace the journey, consult your healthcare provider, and enjoy the many physical and mental benefits that come with an active, diabetes-conscious lifestyle.






Leave a Reply