Polydipsia: A Comprehensive Medical Guide
Polydipsia is the medical term for excessive thirst that cannot be quenched by normal fluid intake. It represents a significant clinical symptom that may indicate underlying medical conditions requiring prompt evaluation and treatment.
Introduction
Thirst is a natural physiological response that helps maintain proper fluid balance in the body. However, when thirst becomes excessive and persistent despite adequate fluid intake, it may signal an underlying medical condition known as polydipsia. This comprehensive guide explores the various aspects of polydipsia, from its definition and causes to diagnostic procedures and treatment options.
Understanding polydipsia is crucial for both healthcare professionals and patients, as it can be an early indicator of serious medical conditions such as diabetes mellitus or diabetes insipidus. Early recognition and proper management of polydipsia can prevent complications and improve quality of life.
What is Polydipsia?
Polydipsia is derived from the Greek words “poly” (meaning many or much) and “dipsia” (meaning thirst). It is defined as an abnormal and persistent feeling of thirst that leads to excessive fluid consumption, typically more than 6 liters per day in adults. Unlike normal thirst, which is satisfied after drinking appropriate amounts of fluid, polydipsia represents an unquenchable thirst that persists regardless of fluid intake.
The condition is often accompanied by polyuria (excessive urination), creating a cycle where increased fluid intake leads to increased urine production, which in turn triggers more thirst. This cycle can significantly impact a patient’s daily activities, sleep patterns, and overall quality of life (source).
Key Characteristics of Polydipsia:
- Persistent thirst lasting days, weeks, or months
- Fluid intake exceeding 6 liters per day
- Inability to satisfy thirst with normal fluid consumption
- Often associated with frequent urination
- May disrupt normal daily activities and sleep
Types of Polydipsia
Medical professionals classify polydipsia into two primary categories based on its underlying mechanism and associated conditions:
1. Psychogenic Polydipsia
Psychogenic polydipsia, also known as primary polydipsia, is associated with psychiatric conditions and represents compulsive water drinking behavior. This type is most commonly observed in patients with mental health disorders, particularly schizophrenia, where it affects approximately 18% of hospitalized patients.
| Characteristic | Description |
|---|---|
| Primary Conditions | Schizophrenia, bipolar disorder, psychotic depression, schizoaffective disorder |
| Mechanism | Disruption of dopaminergic and cholinergic systems affecting thirst regulation |
| Risk Factors | Antipsychotic medications, stress, smoking, chronic psychiatric illness |
| Complications | High risk of hyponatremia and water intoxication |
2. Dipsogenic Polydipsia
Dipsogenic polydipsia, also called compulsory water drinking, occurs when patients consciously consume excessive amounts of water. This type has two main subtypes: habitual polydipsia driven by health-conscious behaviors, and dipsogenic polydipsia secondary to hypothalamic dysfunction.
Habitual polydipsia has become increasingly common in recent years due to popular health and wellness trends promoting excessive water consumption. Patients believe that drinking large quantities of water will improve their health, leading to compulsive drinking behaviors.
Symptoms of Polydipsia
The clinical presentation of polydipsia involves both primary symptoms directly related to excessive thirst and secondary symptoms resulting from fluid and electrolyte imbalances (source).
Primary Symptoms
- Excessive thirst: Persistent, unquenchable thirst despite drinking large volumes of fluid
- Polyuria: Frequent urination, often exceeding 3 liters per day
- Dry mouth (xerostomia): Persistent dryness of the oral cavity
- Frequent drinking: Compulsive need to consume fluids throughout the day and night
- Sleep disruption: Nocturia (nighttime urination) affecting sleep quality
Secondary Symptoms (Hyponatremia)
When excessive water intake overwhelms the kidneys’ ability to excrete water, hyponatremia (low sodium levels) may develop, causing:
- Fatigue and weakness
- Headache
- Nausea and vomiting
- Confusion and disorientation
- Irritability and mood changes
- Muscle weakness and cramps
- Loss of coordination
- Seizures (in severe cases)
Water Intoxication Symptoms
Severe cases may progress to water intoxication, characterized by:
- Severe muscle pain and cramping
- Edema (swelling) of hands, feet, and abdomen
- Altered mental status
- Decreased consciousness
- Respiratory distress
Warning: Severe hyponatremia and water intoxication are medical emergencies requiring immediate hospitalization. Symptoms such as seizures, altered consciousness, or severe confusion warrant immediate medical attention.
Causes of Polydipsia
Polydipsia can result from various underlying medical conditions, medications, and physiological states. Understanding these causes is essential for proper diagnosis and treatment (source).
Endocrine Disorders
Diabetes Mellitus
High blood glucose levels in diabetes mellitus trigger osmotic diuresis, leading to increased urine production and subsequent thirst. This represents one of the classic “three P’s” of diabetes: polydipsia, polyuria, and polyphagia.
Diabetes Insipidus
This condition results from inadequate production or response to antidiuretic hormone (ADH), causing the kidneys to produce large volumes of dilute urine and triggering compensatory thirst.
Hyperthyroidism
Overactive thyroid gland increases metabolic rate and can lead to increased fluid requirements and thirst.
Electrolyte Imbalances
- Hypokalemia: Low blood potassium levels can impair kidney function and increase thirst
- Hypercalcemia: Elevated calcium levels can cause polyuria and secondary polydipsia
- Hypernatremia: High sodium levels trigger thirst mechanisms
Kidney Disorders
Chronic kidney disease, acute kidney injury, and certain genetic kidney disorders can impair the kidney’s ability to concentrate urine, leading to excessive fluid loss and compensatory thirst.
Medications
| Medication Class | Examples | Mechanism |
|---|---|---|
| Anticholinergics | Atropine, scopolamine | Reduce saliva production, increase thirst sensation |
| Diuretics | Thiazides, loop diuretics | Increase fluid loss through kidneys |
| Antipsychotics | Haloperidol, olanzapine | Anticholinergic effects, disrupted thirst regulation |
| Lithium | Lithium carbonate | Nephrogenic diabetes insipidus |
Neurological Conditions
Conditions affecting the hypothalamus, where thirst and ADH regulation occur, can cause polydipsia:
- Brain tumors
- Head trauma
- Infections (encephalitis, meningitis)
- Infiltrative diseases (sarcoidosis, histiocytosis)
- Vascular disorders (strokes affecting hypothalamus)
Psychiatric Disorders
- Schizophrenia
- Bipolar disorder
- Major depressive disorder with psychotic features
- Developmental disorders (autism, intellectual disability)
Diagnostic Tests and Procedures
Diagnosing polydipsia requires a systematic approach combining clinical history, physical examination, and specialized testing to identify underlying causes and differentiate between various conditions.
Initial Assessment
Medical History
Comprehensive history taking includes:
- Onset, duration, and severity of symptoms
- Daily fluid intake quantification
- Urination patterns and volume
- Associated symptoms (weight loss, fatigue, confusion)
- Medication history, including over-the-counter drugs
- Psychiatric history and current mental health status
- Family history of diabetes or kidney disease
- Recent trauma, surgery, or infections
Physical Examination
Physical assessment focuses on:
- Signs of dehydration or fluid overload
- Mucous membrane moisture
- Skin turgor and edema
- Blood pressure and heart rate
- Neurological examination
- Signs of underlying endocrine disorders
Laboratory Tests
Basic Metabolic Panel
- Serum sodium: Essential for detecting hyponatremia or hypernatremia
- Blood glucose: Screening for diabetes mellitus
- Serum osmolality: Assessment of fluid balance
- Creatinine and BUN: Kidney function evaluation
- Potassium and calcium: Electrolyte balance assessment
Urinalysis and Urine Studies
- 24-hour urine collection: Quantifies polyuria (>3L/day indicates polyuria)
- Urine osmolality: Measures urine concentration ability
- Urine specific gravity: Simple concentration assessment
- Urine glucose: Diabetes mellitus screening
Specialized Diagnostic Tests
Water Deprivation Test
The traditional gold standard for differentiating polydipsia causes:
| Test Phase | Procedure | Normal Response |
|---|---|---|
| Pre-test | Baseline weight, serum/urine osmolality | Establish baseline values |
| Deprivation Phase | 8-16 hours without fluid intake | Urine osmolality increases >800 mOsm/kg |
| Desmopressin Challenge | ADH analog administration | Differentiates DI types |
Copeptin Measurement
A newer, more accurate diagnostic approach:
- Baseline copeptin: >21.4 pmol/L suggests nephrogenic DI
- Stimulated copeptin: After osmotic stimulation
- ≥4.9 pmol/L: Primary polydipsia
- <4.9 pmol/L: Central diabetes insipidus
Advanced Testing
- Brain MRI: Evaluate hypothalamic-pituitary region
- CT scan: Assess for structural abnormalities
- Thyroid function tests: Rule out hyperthyroidism
- Hemoglobin A1c: Long-term glucose control assessment
Diagnostic Interpretation
| Condition | Serum Sodium | Urine Osmolality | Response to Desmopressin |
|---|---|---|---|
| Primary Polydipsia | <135 mEq/L | Increases with deprivation | Minimal response |
| Central DI | >147 mEq/L | Remains low despite deprivation | Significant increase |
| Nephrogenic DI | >147 mEq/L | Remains low despite deprivation | Poor response |
Treatment Options
Treatment of polydipsia requires a multifaceted approach addressing both the underlying cause and the immediate complications. The therapeutic strategy varies significantly depending on the etiology, severity, and associated complications (source).
Acute Management
Severe Hyponatremia Treatment
Patients presenting with severe symptomatic hyponatremia require immediate intervention:
- Hypertonic saline (3%): For severe symptoms (seizures, coma)
- Fluid restriction: Limit intake to 1-1.5 L/day initially
- Electrolyte monitoring: Frequent sodium level checks
- Neurological monitoring: Assessment for complications
Critical Warning: Sodium correction must not exceed 8-10 mEq/L per 24 hours to prevent central pontine myelinolysis, a potentially fatal complication.
Cause-Specific Treatment
Diabetes Mellitus
- Blood glucose optimization with insulin or oral hypoglycemics
- Dietary modifications and carbohydrate management
- Regular monitoring and diabetes education
- Treatment of diabetic complications
Diabetes Insipidus
- Central DI: Desmopressin (DDAVP) replacement therapy
- Nephrogenic DI: Thiazide diuretics, amiloride, dietary modifications
- Adequate fluid replacement to prevent dehydration
- Treatment of underlying causes when possible
Psychogenic Polydipsia
Management is challenging due to compulsive nature:
- Behavioral interventions: Structured fluid restriction programs
- Medication adjustment: Reduce anticholinergic medications when possible
- Psychiatric treatment: Optimize antipsychotic regimens
- Environmental modifications: Limited access to water sources
- Patient education: Awareness of risks and complications
(Source)
Pharmacological Interventions
| Medication | Indication | Mechanism | Efficacy |
|---|---|---|---|
| Demeclocycline | Psychogenic polydipsia | Induces nephrogenic DI | Limited evidence |
| Naloxone | Psychogenic polydipsia | Opioid receptor antagonism | Minimal benefit |
| ACE inhibitors | Supportive care | Reduce thirst sensation | Anecdotal reports |
| Clozapine | Schizophrenia with polydipsia | Reduced anticholinergic effects | Some benefit reported |
Behavioral and Supportive Therapies
Fluid Management Programs
- Structured daily fluid allowances
- Monitoring and recording fluid intake
- Gradual reduction in daily fluid consumption
- Reward systems for compliance
Patient Education
- Understanding the condition and its risks
- Recognition of warning symptoms
- Importance of medication compliance
- Regular follow-up scheduling
Monitoring and Follow-up
Laboratory Monitoring
- Daily sodium levels during acute treatment
- Weekly electrolyte panels during stabilization
- Monthly monitoring for stable patients
- Renal function assessment
Clinical Assessment
- Fluid intake and output documentation
- Weight monitoring
- Neurological status evaluation
- Psychiatric symptom assessment
Complications and Risks
Polydipsia can lead to serious and potentially life-threatening complications, particularly when excessive water intake overwhelms the body’s regulatory mechanisms.
Hyponatremia
The most common and dangerous complication of polydipsia is hyponatremia, defined as serum sodium <135 mEq/L.
Pathophysiology
Excessive water intake exceeds the kidneys’ maximum excretory capacity (approximately 12-14 L/day), leading to water retention and dilutional hyponatremia. The condition is exacerbated by factors that impair water excretion:
- Inappropriate ADH secretion
- Reduced solute intake
- Medications affecting kidney function
- Stress and psychiatric symptoms
Clinical Manifestations by Severity
| Sodium Level (mEq/L) | Severity | Symptoms |
|---|---|---|
| 130-135 | Mild | Fatigue, headache, mild confusion |
| 125-130 | Moderate | Nausea, vomiting, muscle cramps, disorientation |
| <125 | Severe | Seizures, coma, respiratory arrest, death |
Water Intoxication
Also known as water poisoning, this condition represents the extreme end of the polydipsia spectrum.
Clinical Features
- Cerebral edema and increased intracranial pressure
- Altered mental status and confusion
- Seizures and focal neurological deficits
- Pulmonary edema and respiratory distress
- Cardiovascular instability
Central Pontine Myelinolysis
A devastating complication resulting from overly rapid correction of hyponatremia.
Risk Factors
- Sodium correction >8-10 mEq/L per 24 hours
- Chronic hyponatremia
- Malnutrition and chronic illness
- Alcoholism
Clinical Consequences
- Permanent neurological disability
- Quadriplegia and pseudobulbar palsy
- Cognitive impairment
- Death in severe cases
Psychosocial Complications
Quality of Life Impact
- Disrupted sleep due to nocturia
- Social isolation and embarrassment
- Inability to participate in normal activities
- Workplace and academic impairment
- Relationship strain
Psychiatric Exacerbation
- Worsening of underlying mental health conditions
- Increased risk of psychiatric hospitalization
- Medication compliance issues
- Development of compulsive behaviors
Long-term Health Consequences
- Chronic kidney disease: From repeated episodes of severe hyponatremia
- Cardiovascular complications: Fluid overload and electrolyte imbalances
- Bone health issues: Chronic electrolyte disturbances
- Cognitive impairment: From recurrent severe hyponatremia episodes
Emergency Situations: Immediate medical attention is required for seizures, altered consciousness, severe confusion, or respiratory distress in patients with known polydipsia.
Prevention and Lifestyle Management
Preventing polydipsia-related complications requires a comprehensive approach involving medical management, lifestyle modifications, and patient education.
Primary Prevention
Early Detection and Management
- Regular screening: Monitor patients at risk (diabetes, psychiatric conditions)
- Medication review: Assess for drugs that may increase thirst
- Patient education: Recognize early warning signs
- Prompt treatment: Address underlying conditions quickly
Risk Factor Modification
- Optimal management of diabetes mellitus
- Appropriate psychiatric medication management
- Regular monitoring of kidney function
- Correction of electrolyte imbalances
Lifestyle Modifications
Fluid Management Strategies
| Strategy | Implementation | Benefits |
|---|---|---|
| Structured intake | Predetermined daily fluid allowances | Prevents excessive consumption |
| Monitoring logs | Daily tracking of intake and output | Increases awareness and control |
| Gradual reduction | Stepwise decrease in daily fluid intake | Allows physiological adaptation |
| Alternative beverages | Sugar-free, electrolyte-containing drinks | May reduce pure water consumption |
Environmental Modifications
- Limited access to water sources when necessary
- Removal of large water containers from living spaces
- Use of measured containers for fluid intake
- Family and caregiver education and involvement
Dietary Considerations
Nutritional Support
- Adequate protein intake: Maintains oncotic pressure
- Appropriate sodium intake: Supports normal osmolality
- Balanced nutrition: Prevents malnutrition-related complications
- Regular meals: Helps regulate thirst patterns
Foods to Consider
- Foods with natural water content (fruits, vegetables)
- Adequate sodium-containing foods
- Avoiding excessive caffeine and alcohol
- Regular, balanced meal timing
Monitoring and Self-Management
Home Monitoring
- Daily weights: Track fluid retention
- Symptom diaries: Record thirst levels and associated symptoms
- Urine output measurement: Monitor for polyuria
- Medication adherence: Ensure consistent treatment
Warning Sign Recognition
Patients and caregivers should be educated to recognize:
- Increasing thirst despite adequate intake
- Rapid weight gain
- Confusion or altered mental status
- Nausea and vomiting
- Muscle weakness or cramps
Support Systems
Healthcare Team
- Primary care physician coordination
- Endocrinology consultation when appropriate
- Psychiatry involvement for psychogenic cases
- Nursing support for monitoring and education
- Dietitian consultation for nutritional management
Family and Social Support
- Caregiver education and training
- Support group participation
- Regular family meetings with healthcare providers
- Emergency response planning
(Source: Cleveland Clinic)
Polydipsia Frequently Asked Questions
Q: What is the difference between polydipsia and normal thirst?
Q: Is polydipsia always a sign of diabetes?
Q: How much water intake is considered excessive?
Q: Can polydipsia be dangerous?
Q: How is polydipsia diagnosed?
Q: What should I do if I think I have polydipsia?
Q: Can polydipsia be treated?
Q: Is polydipsia more common in certain age groups?
Q: Can medications cause polydipsia?
Q: Will polydipsia go away on its own?
Q: How can family members help someone with polydipsia?
Q: Are there any dietary changes that can help with polydipsia?
When to Seek Medical Care
Recognizing when to seek medical attention for polydipsia is crucial for preventing serious complications and ensuring appropriate treatment. The urgency of care depends on the severity of symptoms and associated complications.
Immediate Emergency Care
Seek immediate emergency medical attention (call 911 or go to the emergency room) if experiencing:
Emergency Symptoms:
- Seizures or convulsions
- Loss of consciousness or unresponsiveness
- Severe confusion or disorientation
- Difficulty breathing or chest pain
- Severe muscle weakness or paralysis
- Persistent vomiting preventing fluid intake
- Signs of severe dehydration despite excessive drinking
Urgent Medical Attention (Same Day)
Contact your healthcare provider immediately or visit an urgent care facility for:
- Moderate confusion or memory problems
- Persistent nausea and vomiting
- Severe headaches
- Rapid weight gain (>2-3 pounds in 24 hours)
- Muscle cramps or weakness
- Significant changes in urination patterns
- Blood in urine
- Signs of infection (fever, chills)
Routine Medical Consultation
Schedule an appointment with your healthcare provider within a few days if you experience:
- Persistent thirst lasting more than a few days
- Daily fluid intake exceeding 4-6 liters
- Frequent urination disrupting sleep
- Unexplained fatigue or weakness
- Dry mouth despite adequate fluid intake
- Gradual increase in thirst over weeks or months
- New medications causing increased thirst
Monitoring for Patients with Known Polydipsia
Regular Follow-up Schedule
| Patient Category | Follow-up Frequency | Key Monitoring Parameters |
|---|---|---|
| Newly diagnosed | Weekly for first month | Electrolytes, fluid balance, symptoms |
| Stable on treatment | Monthly for 3 months, then quarterly | Sodium levels, medication compliance |
| Psychogenic polydipsia | Bi-weekly to monthly | Behavioral compliance, psychiatric status |
| High-risk patients | Weekly to bi-weekly | Close electrolyte monitoring |
Red Flag Symptoms for Known Cases
Patients with diagnosed polydipsia should seek immediate care for:
- Sudden worsening of thirst
- New onset confusion or behavioral changes
- Inability to maintain fluid restriction goals
- Signs of medication side effects
- Development of new medical symptoms
Healthcare Provider Selection
Primary Care
Initial evaluation and ongoing management of uncomplicated cases
Specialist Referrals
- Endocrinologist: For diabetes-related polydipsia, hormone disorders
- Nephrologist: For kidney-related causes and complicated electrolyte management
- Psychiatrist: For psychogenic polydipsia and medication management
- Neurologist: For neurological causes or complications
Preparation for Medical Visits
Information to Gather
- Complete medication list (including over-the-counter drugs)
- Symptom diary with onset, duration, and severity
- Fluid intake and output records
- Weight changes
- Previous test results
- Family medical history
Questions to Ask Your Healthcare Provider
- What is causing my excessive thirst?
- What tests do I need?
- How will you monitor my condition?
- What are the treatment options?
- What are the potential complications?
- How often should I have follow-up visits?
- What symptoms should prompt immediate medical attention?
Conclusion
Polydipsia represents a complex medical condition that extends far beyond simple thirst, encompassing a wide range of underlying causes from endocrine disorders to psychiatric conditions. Understanding polydipsia is crucial for early recognition, appropriate diagnosis, and effective management of this potentially serious condition.
The key points emphasized throughout this comprehensive guide include the importance of distinguishing pathological polydipsia from normal thirst, recognizing the two primary types (psychogenic and dipsogenic), and understanding the diverse array of underlying causes. Early identification of polydipsia can prevent serious complications, particularly the life-threatening condition of hyponatremia and water intoxication.
Diagnostic approaches have evolved significantly, with newer methods like copeptin measurement offering improved accuracy over traditional water deprivation tests. However, the diagnostic process remains complex, requiring careful clinical assessment, appropriate laboratory testing, and sometimes specialized procedures to identify underlying causes accurately.
Treatment strategies must be individualized based on the underlying etiology, with particular attention to managing acute complications while addressing root causes. The challenges in treating psychogenic polydipsia highlight the need for multidisciplinary approaches involving psychiatrists, behavioral therapists, and medical specialists working together.
Prevention and ongoing management require a comprehensive approach that includes patient education, regular monitoring, lifestyle modifications, and strong support systems. Family members and caregivers play crucial roles in recognizing warning signs and supporting treatment compliance, particularly in cases involving psychiatric conditions.
Potential Complications of Polydipsia
The potential complications of polydipsia, including severe hyponatremia and central pontine myelinolysis, underscore the importance of careful medical management and appropriate correction of electrolyte imbalances. Healthcare providers must balance the need for treatment with the risks of overly rapid intervention.
Looking forward, continued research into the pathophysiology of polydipsia, particularly psychogenic forms, may lead to more effective treatments. The development of more precise diagnostic tools and targeted therapies offers hope for improved outcomes for patients suffering from this challenging condition.
For patients and families dealing with polydipsia, the key message is that effective management is possible with proper medical care, patient education, and adherent follow-up. While the condition can be serious, understanding the warning signs, following treatment recommendations, and maintaining regular medical care can prevent complications and improve quality of life.
Healthcare providers should maintain a high index of suspicion for polydipsia in at-risk populations, including patients with diabetes, psychiatric disorders, and those taking medications known to affect thirst or kidney function. Early intervention and appropriate management can significantly improve outcomes and prevent the serious complications associated with this condition (source).
Key Takeaways:
- Polydipsia is excessive thirst that cannot be satisfied by normal fluid intake
- Multiple underlying causes require thorough evaluation and individualized treatment
- Complications can be life-threatening but are preventable with proper care
- Multidisciplinary management approaches offer the best outcomes
- Patient education and family support are essential components of successful treatment
- Regular monitoring and follow-up care are crucial for preventing complications
This comprehensive understanding of polydipsia empowers both healthcare providers and patients to recognize, evaluate, and manage this complex condition effectively, ultimately leading to better health outcomes and improved quality of life for those affected.
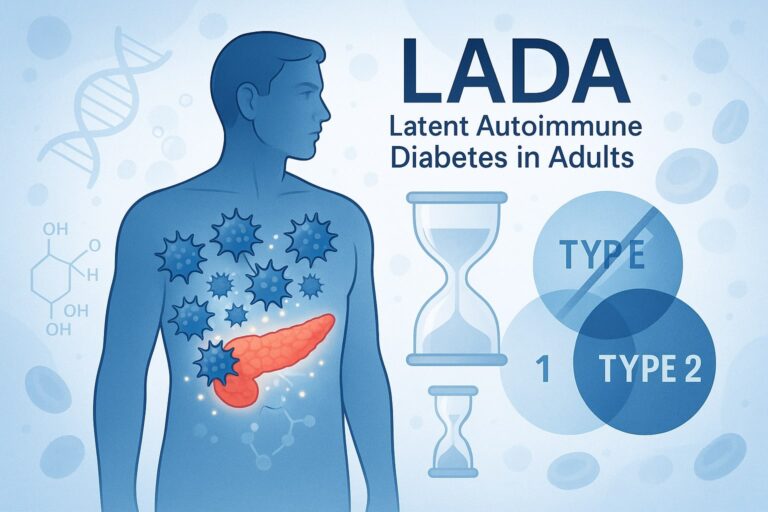
Have you been feeling persistently hungry? Read our piece on hyperphagia. Get more solutions for diabetes, read about the Somogyi effect, reactive hypoglycemia and LADA Diabetes.





Leave a Reply