Blood Sugar Management
For many people with diabetes, blood sugar management can sometimes feel like juggling multiple tasks at once. You might wonder what counts as a healthy range, how to handle post-meal spikes, or when to worry about low readings. The good news is that a few well-organized charts and a clear understanding of your glucose numbers can simplify this process. In this ultimate guide, you’ll find helpful insights into normal ranges, daily tracking, and lifestyle tips so you can keep your levels under control and feel more confident day to day.
Blood Sugar Management Basics
Blood sugar, also called blood glucose, is the body’s main source of energy. You get it from foods that contain carbohydrates, including bread, fruits, and even yogurt. According to MedlinePlus, when glucose rises after meals, your pancreas releases insulin to help shuttle that glucose into cells for energy.
If your body doesn’t produce enough insulin or resists the insulin it does make, your blood sugar may stay too high. This can lead to issues like fatigue, blurred vision, and long-term health complications. On the flip side, blood sugar dropping too low may cause dizziness or shakiness. Finding the sweet spot requires consistent awareness of your glucose levels.
Use Charts For Tracking
Having a simple chart in front of you is like having a roadmap. Instead of guessing whether you’re in a healthy range, you can quickly compare your results with ideal targets. For more details, you can check out blood sugar charts on our site to see typical ranges.
Sample Blood Sugar Chart
Below is a quick-reference table that many people find useful for their blood sugar management. Remember, these are general guidelines, and your personal targets may differ based on your doctor’s advice.
| Time of Day | Typical Range (Non-Diabetics) | Common Target (Diabetics) |
|---|---|---|
| Fasting (Morning) | 70–99 mg/dL | 70–130 mg/dL |
| Pre-Meal | 70–99 mg/dL | 70–130 mg/dL |
| Post-Meal (2 hours) | < 140 mg/dL | < 180 mg/dL |
| Bedtime | 90–120 mg/dL | Individualized by your doctor |
(Adapted from ranges suggested by CDC and other expert sources.)
Fasting vs. Post-Meal
Fasting levels typically measure how your body handles blood sugar overnight. Post-meal levels, on the other hand, show how your system copes with sugar from food. Monitoring both can guide you in tweaking meal choices. If you want more specifics, take a look at normal blood sugar levels and post-meal blood sugar levels.
Recognize High And Low Blood Sugar Patterns
If you frequently spot concerns on your chart, it’s time to step back and see whether your blood sugar is running too high or too low. Learning the classic warning signs can help you act quickly.
Frequent Highs
High blood sugar (hyperglycemia) often comes with increased thirst, frequent bathroom breaks, and unexplained fatigue (MedlinePlus). When you notice your readings inching above 180 mg/dL regularly, consider reviewing your meal plan or consulting your healthcare provider. Chronic hyperglycemia can harm your blood vessels, increasing the risk of heart problems and infections.
Frequent Lows
Low blood sugar (hypoglycemia) can pop up if you skip meals, overexercise, or take too much diabetes medication. You might feel sweaty, shaky, dizzy, or confused. Levels under 70 mg/dL are generally considered too low, and you’ll want to address them right away with a quick source of carbs—like fruit juice. For deeper insight into hypoglycemia signals, visit high and low blood sugar symptoms.
Track And Adjust Daily
Daily tracking can be as basic as writing down numbers in a notebook or as high-tech as using a continuous glucose monitor (CGM). Tools like a CGM can measure your blood sugar every few minutes and send updates right to your phone or smartwatch (CDC).
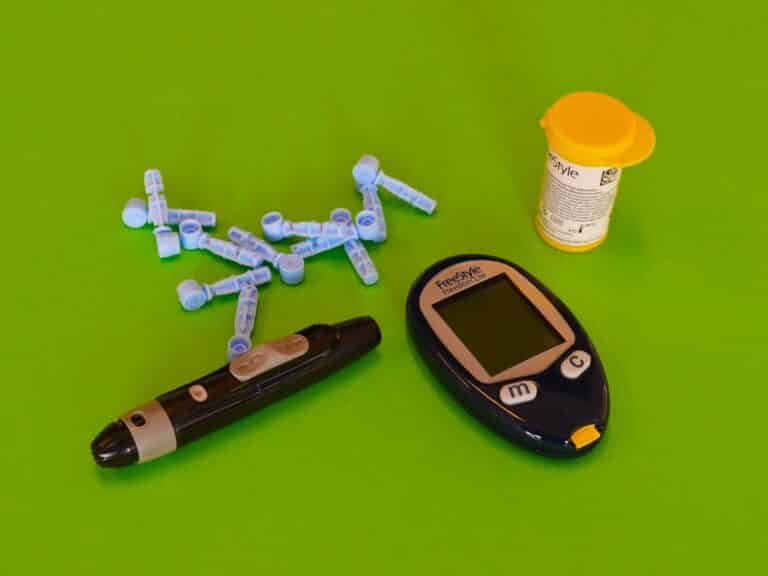
Using A Glucose Meter Or CGM
- Glucose Meter: Prick your finger, place a drop of blood on a test strip, and get a reading in seconds.
- CGM System: Insert a small sensor under your skin. It monitors glucose automatically, lowering the need for finger-prick tests.
By comparing your day’s numbers to the chart above, you’ll see patterns emerge. Maybe mornings are consistently higher, or post-meal readings spike after certain foods. Adjust meals, medication, or exercise accordingly to master your blood sugar management.
Daily Record Strategies
- Note your readings in a journal or app four to six times a day.
- Track patterns in relation to your meals. For instance, record breakfast details if you see a high mid-morning reading.
- Log unusual circumstances, like stress or sickness, which can temporarily skew glucose results (American Diabetes Association).
Adopt Healthy Habits
Healthy habits go hand in hand with effective blood glucose regulation. If you’re consistently mindful—without being overly rigid—these small changes can make a real difference.
Nutrition And Carb Counting
Carbohydrates have the biggest impact on your blood sugar. According to Healthline, counting your carbs helps you better predict how meals influence your readings. Focus on whole grains, fruits, and veggies for balanced energy, and aim to space your carbs evenly throughout the day.
- Include lean proteins like chicken, fish, or beans for longer-lasting fullness.
- Avoid sugary drinks and snacks that spike blood sugar quickly.
- Use your chart to understand which foods nudge your numbers upward.
Water And Hydration
Drinking enough water helps flush out excess sugar and prevent dehydration. If you’re not a fan of plain water, try zero-calorie flavored waters or herbal teas (as long as they don’t have added sugar). MD Anderson points out that proper hydration can help your kidneys filter out and eliminate excess glucose.
Exercise And Blood Sugar
Most forms of aerobic exercise will lower blood sugar, while certain high-intensity workouts or heavy weight training can briefly raise it (American Diabetes Association). If you notice your sugar rising after intense sessions, try gentler activities like brisk walking or moderate cycling to find what works best for you.
- Aim for at least 150 minutes per week of moderate activity (like walking).
- Include strength exercises to build muscle, which burns glucose more efficiently.
- Check your numbers before and after workouts to see how exercise affects you.
Final Thoughts And Next Steps
Using charts is one of the easiest ways to simplify your day-to-day management routine. You get a clear visual snapshot that helps you catch high or low trends before they become a problem. Pair that with mindful eating, plenty of water, and consistent exercise, and you’ll be well on your way to more stable readings. Also, if you’d like to calculate your A1C or average blood sugar level, try our A1C calculator for instant results.
Curious about specific ranges or what might be throwing your numbers off? See our blood sugar charts for a closer look at typical targets, or check out resources about normal blood sugar levels, post-meal blood sugar levels, and high and low blood sugar symptoms. You deserve to feel confident in your diabetes care, and these tools can make each day a little more feasible for your blood sugar management.
Give one or two of the strategies above a try, and see how your numbers respond. If you spot any concerning trends, reach out to your healthcare team. With a bit of experimentation and consistent monitoring, you’ll discover what works best for you. Remember, we’re all unique, and your body deserves a custom approach that keeps you feeling your best.






Leave a Reply