Implant Reverses Type 1 Diabetes in Mice by Delivering Beta Cells
Previously Published on Medical News Today – New research uses stem cells and a tiny device, the implant reverses type 1 diabetes in mice.
- Insulin-secreting beta cells can reverse type 1 diabetes in mice.
- Introducing these cells without triggering the immune system has been a critical challenge.
- Researchers have developed an apparently safe, functional device for delivery of the beta cells, while stressing that more research is needed to help in the treatment of type 1 diabetes.
Some of the most favorable alternative sources for diabetes cell replacement therapy are human stem cells. However, a critical challenge has been finding a safe, effective means to introduce replacement cells that normalize blood sugar levels without triggering the body’s natural immune response.
Researchers at the Washington University School of Medicine in St. Louis, MO, and Cornell University in Ithaca, NY, have collaborated to develop a tiny implant that successfully delivers insulin-secreting cells, or beta cells, into mice with diabetes, without the need for immunosuppressive drug treatment.
The study appears in the June 2 issue of Science Translational Medicine.
The autoimmune response
Beta cells are unique cells in the pancreas that produce, store, and release insulin. Dr. Jeffrey R. Millman, one of the researchers, had previously participated in research that led to a method to make pluripotent stem cells — that is, cells that can give rise to several different cell types — and then grow those cells into insulin-secreting beta cells.
“We can take a person’s skin or fat cells, make them into stem cells, and then grow those stem cells into insulin-secreting cells,” said Dr. Millman. “The problem is that in people with type 1 diabetes, the immune system attacks those insulin-secreting cells and destroys them.”
Introducing new insulin-producing cells can re-trigger the autoimmune disease process that originally destroyed beta cells in the pancreas of someone with type 1 diabetes. Even though there are drugs available that suppress the immune system, researchers note that using these drugs makes patients vulnerable to infections.
A NICE device
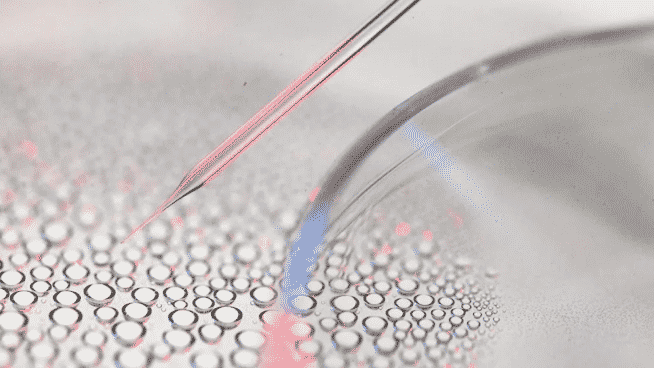
Scientists have tried several implants in recent years with varying levels of success. It is vital that the device has small enough openings to prevent the invasion of immune cells while being large enough to take in nutrients and oxygen and release the insulin.
The team of researchers developed a nanofiber-integrated cell encapsulation, or NICE, device. After filling NICE implants with stem cell-derived, insulin-secreting beta cells, the researchers inserted the devices into the abdomens of mice with chemically induced diabetes.
Diabetes correction occurred within 1 week of the implantation of the NICE devices. The cells in the implants continued to secrete insulin, control blood sugar, and reverse diabetes in the treated mice for up to 200 days with no drugs administered to suppress their immune systems.
The Goldilocks zone
“The device, which is about the width of a few strands of hair, is microporous — with openings too small for other cells to squeeze into — so the insulin-secreting cells consequently can’t be destroyed by immune cells, which are larger than the openings,” said Dr. Millman.
“With this device, we seem to have made something in what you might call a Goldilocks zone, where the cells could feel just right inside the device and remain healthy and functional, releasing insulin in response to blood sugar… Share on XCo-researcher Dr. Minglin Ma added: “The combined structural, mechanical, and chemical properties of the device we used kept other cells in the mice from completely isolating the implant and, essentially, choking it off and making it ineffective. The implants floated freely inside the animals, and when we removed them after about 6 months, the insulin-secreting cells inside the implants still were functioning. And, importantly, it is a very robust and safe device.”
The soft but tough NICE device is made from a porous medical grade thermoplastic material. It can be implanted and retrieved laparoscopically. The safety of the implant was confirmed through the continuous containment and activity of the beta cells over the study period.
Stem cell-derived beta cellsTrusted Source hold great promise for treating type 1 diabetes by providing a nearly unlimited number of insulin-secreting cells. The low complexity design, relatively easy fabrication, and balance of safety and function make the NICE device an ideal candidate for future development and eventual clinical applications.
Other research in which an implant reverses type 1 diabetes, as well as improved insulin news.
Previously Published on Medical News Today