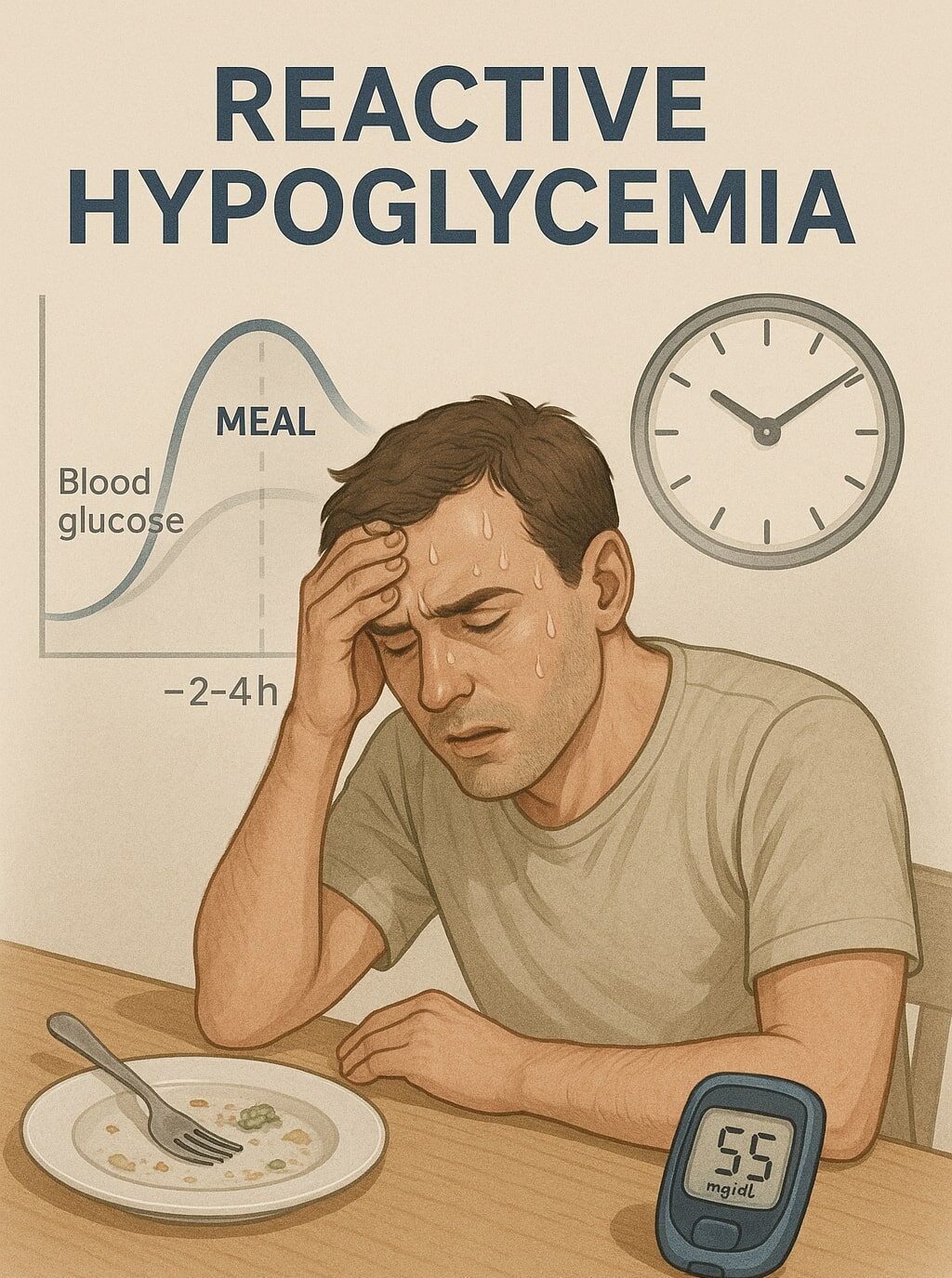
Reactive Hypoglycemia: Symptoms, Causes and Treatments
Have you ever felt shaky or anxious a couple of hours after a meal? That curious drop in blood sugar might point to reactive hypoglycemia (also called postprandial hypoglycemia). This ultimate guide walks you through what it is, why it happens, and how you can stay in control. By the end, you’ll have a clear roadmap for preventing those unwelcome sugar crashes and feeling more balanced every day.
What is Reactive Hypoglycemia?
Reactive hypoglycemia happens when your blood glucose dips within about four hours after eating. Unlike low blood sugar tied to diabetes, this condition can happen even if you don’t have a history of diabetes. Researchers suggest it might be the body producing extra insulin in response to carb-heavy meals, leading to a quicker-than-normal drop in glucose levels (Mayo Clinic, Cleveland Clinic).
Think of it like overshooting the mark: your body wants to regulate your blood sugar after your meal, but it goes too far. This can produce some surprising symptoms, including jitters, sweating, or even a sense of panic. While it may feel scary at first, understanding it is often the first step in feeling better.
Recognize Common Symptoms of Reactive Hypoglycemia
How do you know if you’re experiencing this condition? Symptoms usually pop up a few hours after you eat, especially if you had simple carbs (like pastries or white bread).
- Shakiness and sweating
- Heart palpitations or racing heartbeat
- Sudden hunger (similar in intensity to polyphagia)
- Anxiety or irritability
- Dizziness or lightheadedness
You might notice you get frantic for food or feel a sense of weakness that’s tough to ignore. If these signs appear consistently, it’s a good idea to monitor your blood sugar or talk to your doctor about a possible mixed-meal tolerance test (MMTT).
Explore Main Causes of Reactive Hypoglycemia
Where does this blood sugar free-fall come from? Many factors can contribute, but here are some of the most common:
- Excess Insulin Production
After a carb-heavy meal, your pancreas produces insulin to manage your rising blood glucose. Sometimes, it overreacts and pumps out too much, causing that afternoon crash. - Meal Composition
Foods like white rice, sweet pastries, and white bread break down quickly, spiking blood sugar and then dropping it just as fast. - Bariatric Surgery
Certain digestive surgeries speed up sugar absorption, nudging the pancreas to release extra insulin. That can set you up for mid-morning or mid-afternoon slumps (Cleveland Clinic). - Underlying Conditions
Tumors, metabolic issues, or even the somogyi effect (more commonly discussed in diabetes) could also play a role. Although rarer, it’s worth investigating medical causes if lifestyle changes don’t help.
Learn The Diagnosis Process
Not every sugar crash is a sign of reactive hypoglycemia, so how do you confirm what’s going on?
- Document Symptoms
Track when you feel shaky or fatigued. Note what you ate and when your symptoms appeared. - Blood Sugar Checks
Your healthcare provider may recommend checking blood glucose while you’re experiencing symptoms. A reading below 70 mg/dL can be a red flag (WebMD). - Mixed-Meal Tolerance Test (MMTT)
This test involves drinking a special blend of protein, fats, and sugar to provoke insulin release. Your glucose levels are then measured over several hours to see if they plummet unexpectedly (Drugs.com).
Putting these clues together helps your doctor figure out whether you’re dealing with a true hypoglycemic episode or just a normal dip in energy.
Implement Effective Treatments for Reactive Hypoglycemia
Good news: you can often manage this condition through lifestyle tweaks or mild medical support. Let’s walk through your main options.
1. Lifestyle Modifications
- Small, Frequent Meals
Try eating every 3-4 hours. Smaller meals keep blood sugar more stable and prevent massive insulin surges. - Balanced Plates
Pair carbs with protein or healthy fats. For instance, steel-cut oatmeal topped with nuts or seeds can bring more stable energy than a quick bowl of sugary cereal (Healthline). - Prioritize Complex Carbs
Swap simple starches for whole grains, beans, and vegetables that digest more slowly. - Avoid Sugary Drinks
Sodas or fruit juices can spike your glucose and trigger a fast crash. - Bedtime Snack
A small portion of protein and complex carbs before bed helps keep blood sugar on a more even keel overnight.
2. Medical Interventions
For persistent cases, doctors sometimes recommend metformin to improve insulin sensitivity (Frontiers in Endocrinology). In rare situations, a GLP-1 analogue can be added, especially if you’ve had gastric surgery. These medications lower insulin peaks and keep your post-meal blood sugar more stable.
3. Tech and Monitoring
Flash glucose monitoring can give you early warnings of a potential drop. If you’re someone who experiences frequent dips, tracking your glucose trends in real time can be empowering and help you prevent more severe episodes (Frontiers in Endocrinology).
4. Address Underlying Causes
If your tests show additional concerns (like insulinoma or other metabolic disorders), treating those conditions may resolve the hypoglycemia. In other words, always check in with your healthcare team if your blood sugar doesn’t respond to typical lifestyle changes.
FAQs About Reactive Hypoglycemia
- How Quickly Do Symptoms Show Up After a Meal?
Typically, you may notice signs of low blood sugar within two to four hours after eating, especially if the meal was high in simple carbs. - Is Reactive Hypoglycemia Related to Diabetes?
It can occur in people with diabetes or in those without any diabetes diagnosis. For non-diabetic individuals, the mechanism is often excessive insulin release after meals. - What’s the First Step if I Suspect It?
Keep track of your symptoms, then discuss them with a healthcare professional. You may be asked to perform a mixed-meal tolerance test or check your blood sugar during an episode. - Can I Exercise If I Have Hypoglycemic Episodes?
Absolutely, but plan carefully. Eat a balanced snack before working out and consider monitoring your glucose until you understand how exercise affects you. - Are There Any Conditions That Mimic Reactive Hypoglycemia?
Sometimes severe hunger or hyperphagia can look similar, and emotional stress can cause shaky feelings. That’s why documenting blood sugar readings and symptoms is so vital in pinpointing the real cause.
By making a few strategic changes and staying in tune with your body, you can tame reactive hypoglycemia and keep those post-meal crashes in check. It’s all about knowing your triggers, adjusting your meals, and talking to the right experts when necessary. You’ve got this!
If you’ve got extreme thirst that can’t be quenched, check out our piece on Polydipsia.




Leave a Reply